Sjögren’s syndrome
A systemic autoimmune rheumatic disorder
Sjögren’s syndrome is a condition striking parts of the body that produce fluids, e.g. tears and saliva, through focal lymphocytic infiltrations of salivary and lachrymal glands. Other parts of the body, such as nerves and joints, can also be affected. Extra-glandular manifestations such as fatigue, pain, and depression are observed in 50% of patients. Sjögren’s syndrome usually starts in patients aged 40-60, more commonly in women.
Sjögren’s syndrome strikes an estimated population of more than a million patients worldwide, predominantly post-menopausal women. Available therapeutic options are symptomatic. There is no curative treatment available.
Regulation of IFN-stimulated genes may confer a causal treatment option.
Systemic scleroderma
A rare auto-immune disease of skin and connective tissue
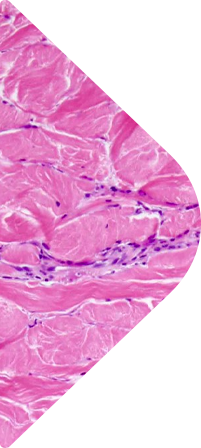
Scleroderma is a group of rare diseases that involve the hardening and tightening of the skin and connective tissues.
While in some patients scleroderma only affects the skin, patients struck with systemic scleroderma also see harm in blood vessels, internal organs and the digestive tract. This is due to the excessive production and accumulation of collagen in skin and internal organs (fibrosis) and injuries to small arteries (vasculopathy).
Scleroderma is a high morbidity, high mortality condition that affects women more often than men (3:1 ratio) and most commonly occurs between the ages of 30 and 50. An estimated 1,000,000 patients live with scleroderma worldwide.
While there is no cure for scleroderma, a variety of treatments can ease symptoms and improve quality of life such as immune suppression for skin and lung fibrosis improves survival (88% survival at 10 years). Yet, substantial non-lethal complications (arthritis, myalgia) remain.
As the fibrotic process is driven by ISGs, increased gene expression of TBK1, IRF3, IRF7 and STAT1 in whole blood and pTBK1 in pDCs are observed in IFN-positive systemic scleroderma patients. Again in past studies treatment with BX795 of these PBMCs downregulated ISG expression, indicating that TBK1 could be a treatment target.
Dermatomyositis
A rare inflammatory muscle and skin disease
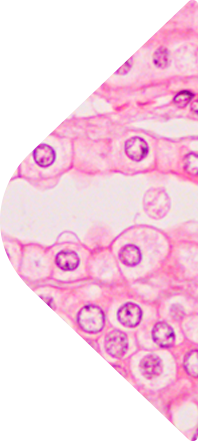
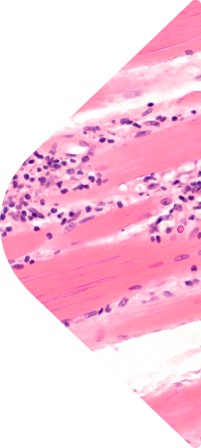
Dermatomyositis is an uncommon inflammatory disease marked by muscle weakness and a distinctive skin rash.
The condition can affect adults and children. In adults, dermatomyositis usually occurs in the late 40s to early 60s. In children, it most often appears between 5 and 15 years of age. Dermatomyositis affects females more than males. 50% of patients have moderate to severe itching, progressing muscle weakness, and specific histological features.
The condition is due to chronic and sustained inappropriate intracellular production of type I IFN-inducible proteins, specifically MxA and ISG-15.
Dermatomyositis strikes an estimated population of 100,000 patients worldwide, predominantly post-menopausal women. There’s no cure for dermatomyositis, but periods of symptom improvement can occur.
In past studies TBK1 inhibition (BX795) showed efficacy in decreasing ISGs expression in PBMC (Gitiaux, 2020), making TBK1 inhibition a potential causal treatment for dermatomyositis.
Interferonopathies
A family of rare genetic disorders manifesting in type I IFN up-regulation
Interferonopathies are a group of rare to ultra-rare severe genetic disorders, many of which manifest in early childhood. They are characterized by the up-regulation of type I IFN. Out of a dozen interferonopathies, two are described in more details below.
- Aicardi-Goutières Syndrome (AGS): inherited inflammatory-mediated encephalopathy characterized by increased type I IFN activity and upregulation of IFN-stimulated genes (ISGs).
- STING associated vasculopathy with onset in infancy (SAVI): a rare, genetic autoinflammatory disorder, type I interferonopathy due to constitutive STING (STimulator of INterferon Genes) activation, characterized by neonatal or infantile onset systemic inflammation and small vessel vasculopathy resulting in severe skin, pulmonary and joint lesions.
Interferonopathies strike an estimated population of 10,000 patients worldwide, young children in particular. When available, treatments for interferonopathies are symptomatic or palliative at best.
Direct down-regulation of type I IFN could confer a causal treatment option.
GvHD
Graft-versus-host disease (GvHD)
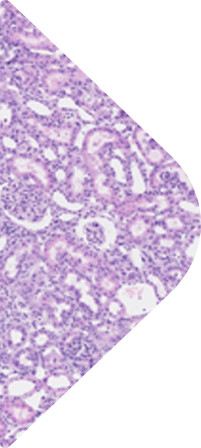
Graft-versus-host disease (GvHD) is a syndrome, characterized by inflammation and selective damage in different organs such as the liver, skin (rash), mucosa, and the gastrointestinal tract.
It might occur after an allogeneic bone marrow or stem cells transplant. In 30% to 50% of allogeneic transplant, the donated bone marrow or stem cells view the recipient’s body as foreign, and the donated cells/bone marrow attack the body.
The two types of GvHD are acute and chronic. In Acute GvHD, the diseases declares in the first 100 days post transplant.
The most important factor to increase the development of aGvHD is the donor/recipient HLA (human leukocyte antigen) match. The advanced age of either the donor or the recipient may also have a role.
While GvHD can deeply impact the quality of life by attacking the normal cells, a similar immune response is also seeked to destroy any surviving cancer cells. This is called the graft versus tumor effect (GvT). Patients who develop GvHD have lower disease relapse rates.
It has been proposed that modulation of the ICOS signalization such as what TBK1 inhibitors can do, could opportunistically block the deleterious mechanism active in GvHD, while not perturbating the Graft versus tumor effect.

